More on antimicrobial resistance – sorry!
At the risk of being boring, I came across two articles, which were of interest, in the ongoing debate over veterinary use of antimicrobials.
The first was looking at antimicrobial resistance patterns in Hungarian Escherichia coli from man and animals (Szmolka et al, 2012) and the second of clinical importance regarding resistance in Actinobacillus pleuropneumoniae isolates in Italy.
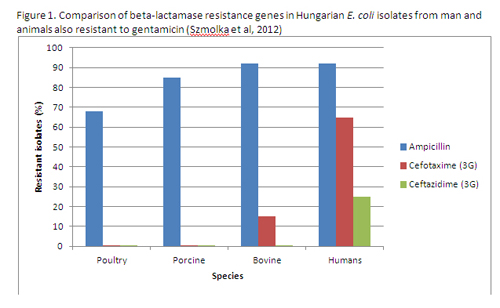
Escherichia coli are ubiquitous organisms primarily living in the gut but can cause clinical infections, in pigs primarily enteritis but can invade the blood stream and cause coli-septicaemia, which results in death often in piglets. In man they can cause urinary tract infections, and blood and wound infections. Isolates from poultry, pigs and cattle both from intestines and clinical material were screened for the presence of gentamicin (aminoglycoside antibiotic) resistance and these isolates carrying this gene were compared with human isolates also carrying the gene and other multi-resistance genes. They used a new microarray system, developed in the UK, which identifies the individual genes (bits of DNA) that cause resistance (see Figure 1)
Figure 1. Comparison of beta-lactamase resistance genes in Hungarian E. coli isolates from man and animals also resistant to gentamicin (Szmolka et al, 2012)
They showed that ampicillin (penicillin/ beta-lactamase antibiotic) was commonly co-resistant with gentamicin across all species with isolates being 68-92% resistant. But when it came to the important 3rd generation cephalosporins (cefotaxime and ceftazidime), which are widely used in man, there was some bovine isolates resistant to cefotaxime but none in poultry or pig isolates. In man the resistance was 65%. Against ceftazidime there was no resistance reported in animals but 25% in man.
The authors thought that the common combined use of gentamicin and beta-lactam antibiotics in hospitals for treating serious bacterial infections in humans has lead to the selection of
corresponding resistance genes in man rather than in animal E. coli strains. That is, it has come from human use rather than use in animals.
Of concern though was the report of Vanni et al (2012) regarding the susceptibility of A. pleuropneumoniae to the beta lactam type of antibiotics (see Figure 2).
Figure 2. Resistance development by Italian A. pleuropneumoniae to various beta-lactam antibiotics with time (Vanni et al, 2012)
Over the last 15 years, resistance to amoxycillin has developed up to 80% in some years. Normally, this resistance is due to beta-lactamase enzymes being produced by the bacteria, which breaks down the basic penicillin or beta-lactam ring and stops the antibiotic working. A recent survey of EU A. pleuropneumoniae isolates put the resistance level at about 5% (Felmingham, 2009), so these Italian results are unusually severe. Interestingly, much of the resistance can be neutralised by the combination of amoxycillin and the beta-lactamase inhibitor, clavulanic acid, which binds to the beta-lactamase enzyme preventing the inhibition of the antibiotic. The resistance level drops substantially to below 10%. Resistance to cephalexin, a first generation cephalosporin (cephalexin) is also very high peeking at over 50%, which is a surprise. The 3rd generation cephalosporin (ceftiofur) resistance is also low, below 15%, clearly demonstrating that it is resistant to the more common cephalosporinases and other beta-lactamases, hence its popularity.
There is a major political push going on in the EU to restrict the use or even ban the use of 3rd generation cephalosporins in veterinary medicine but this data shows that they are highly important also in veterinary medicine, as A. pleuropneumoniae can be lethal in pigs. It also highlights the benefits and clinical importance of products, which contain beta-lactamase inhibitors, such as clavulanic acid, to keep the beta-lactam antibiotics working.
Third generation cephalosporin resistance in man would appear to be induced primarily by human medical use and not from animals, according to the Hungarian data. However, the data from Italy demonstrates that we must not be complacent about the use of antibiotics and must start using them responsibly and wisely.











