Bacteria and antimicrobials – a concise compendium
Beta-lactamases, inhibitory concentrations, ESBLs, gram-positive bacteria – these concepts are frequently addressed in Pig Progress, but does each pork producer know exactly all the ins and outs around antimicrobials? Once and for all – here are the answers.
Antimicrobial compounds have been available for both human and veterinary medicine for almost 70 years and indeed we have benefitted from their use during this period so that common infections no longer kill us or animals. As a result, we have been able to advance public health, hospital treatment and surgery as well as animal health and production to a very high degree. This reliance, almost dependence, on these drugs has allowed us to progress dramatically but have they now become a substitute for poor hygiene in our hospitals and care homes, lack of personal care concerning transmission of infections on the human side? Has it also led to overcrowding and overstocking on farms and lack of attendance to basic biosecurity, such as disease carrying status of animals, personnel and traffic coming on to the farm and just living with the resulting diseases?
As a result we are facing major issues over resistance development in both human and to a lesser extent veterinary medicine. At the same time, we have seen a drop off in investment to develop new compounds to help replace the ones that are no longer effective, especially in human medicine. The purpose of this article is to look at how antimicrobials work and try to understand the dilemmas that are facing the regulators over their use in both veterinary and human medicine.
Definition of antibiotics and antimicrobials
On purpose this article uses the word antimicrobial first in this article, as it covers any product that works against microbes e.g. bacteria, mycoplasma, fungi, protozoa, viruses, both naturally occurring compounds (like penicillins and tetracyclines) and synthetic ones (like the sulphonamides and fluoroquinolones).
The naturally occurring compounds are produced commercially by fermentation processes and these are termed antibiotics. These are active against many bacteria and mycoplasma but also fungi and protozoa like coccidia.
Antibiotics can be manipulated by the addition of side chains or slightly changing their chemical structure to enhance their relative activity or spectrum of activity against different types of bacteria. The classic example is the change of penicillin to ampicillin or amoxycillin, which are semi-synthetic antibiotics.
Most of the interest regarding resistance is focussed currently on bacteria. The term antibacterial covers both antibiotics and antimicrobials in general and is more specific to our concerns. There are also antivirals, antifungals, anticoccidials etc. and these are also specific to the type of microbe that they attack. This article will focus mainly on antibacterials.
How antibacterials function
Some antibacterials act on bacteria and inhibit their growth and are termed bacteriostatic. The tetracyclines, the most widely used antibacterials in veterinary medicine (45% in the UK), are a good example of this. A functioning immune system is important with these drugs, to control or eliminate the infection and to build up an immune response. Some compounds are bacteriostatic at low concentrations but as the concentration rises they can become bactericidal e.g. kill the bacteria directly. Florfenicol and the pleuromutilin, tiamulin, are examples of these against certain bacteria and mycoplasma. Other antibacterials are primarily bactericidal e.g. the fluoroquinolones, like enrofloxacin and marbofloxacin and the aminoglycosides like neomycin, apramycin, gentamicin and amikacin and these act directly on the bacteria and kills them. The killing rate is dependent on the concentration that is achieved at the site of infection, so they are called concentration-dependent. Penicillin and cephalosporins are also bactericidal but they are considered time-dependent in their mode of action, so the bacteria need a longer exposure to the drug for it to have an effect. As these compounds kill the bacteria, they are much liked by the medical profession, as they often encounter infections in patients that have damaged immune systems from HIV, radio- and chemotherapy, or have suppressed immunity following transplants etc., to prevent organ rejection. The young and the old are also more prone to infections. Immunosuppression is less important in veterinary medicine but some viruses can suppress the immune system in pigs like PRRSv and PCV2 and we are working with young, growing animals all the time.
Susceptibility
The susceptibility of the bacteria to a compound is determined in vitro by growing the bacteria in different concentrations of the antibacterial (see also illustration). Where the bacteria stop growing that is termed the minimum inhibitory concentration (MIC) and where all the bacteria are killed that is the minimum bactericidal concentration (MBC) e.g. the pharmacodynamics of the drug. The MIC and MBC can be quite different for the bacteriostatic drugs but almost identical for the bactericidal drugs due to their mode of action. From these figures we can then relate them to achievable drug concentrations in the blood, other fluids or tissues or even gut contents (pharmacokinetics of the drug) to see if they are likely to be effective and at what dose. Many laboratories monitor large numbers of isolates of bacteria and when these results are put together their susceptibility patterns and resistance patterns can be identified (see Figure 1) and correlated with the drug concentrations.
Classifying bacteria
There are many different species or types of bacteria. A common way of differentiating them was by culturing them and staining them. Some bacteria like to grow in air or oxygen and are called aerobic bacteria, e.g. Streptococcus, Staphylococcus, Actinobacillus, Pasteurella and some do not need oxygen and are termed anaerobic, Clostridium perfringens and Brachyspira hyodysenteriae would be examples of these and tend to be found in the large intestine. Others like reduced oxygen – micro-aerophilic – like Lawsonia intracellularis and live at the end of the small intestine in the ileum mainly. Other bacteria, like Escherichia coli and Salmonella, can live in both environments.
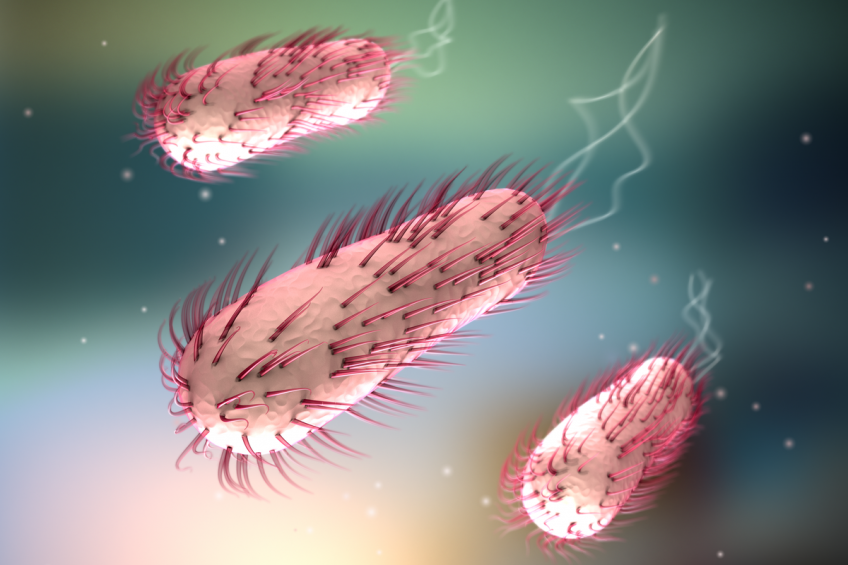
A close-up of Salmonella bacteria.
Another method of classifying bacteria is by staining them using a Gram stain. Gram positive (G +ve) stain dark blue and can be both aerobic and anaerobic e.g. Staphylococcus, Clostridium and Gram negative (G –ve) which stain pink to red and also can be aerobic and anaerobic e.g. Pasteurella, E. coli and Brachyspira.
The shape of the organism is also helpful, Staphylococcus is round in shape (coccus), E. coli is a rod shape and Brachyspira is a spiral shape.
Antibacterial differentiation
The penicillins or beta-lactam antibiotics (because they have a basic beta-lactam ring in their core structure – see Figure 2) offer a very interesting example of how antibacterials were developed and differentiated. They have been very successful and account for 68% of human used antibacterials in the UK. Penicillin use was discovered as far back as 1928 but was not commercialised until much later in the forties. It is a relatively narrow-spectrum antibacterial with activity against Gram +ve bacteria such as Staphylococci and Clostridium as well as some Gram –ve ones such as Pasteurella and Haemophilus but not E. coli or salmonella.
By changing the side chain they made the aminobenzyl penicillins ampicillin and amoxicillin in the sixties, which had an extended/expanded spectrum to include E. coli and Salmonella and have become the mainstays of routine human antibiotic therapy to this day. Bacteria are very clever and want to survive and as a result they produced enzymes to counter the attack by the antibacterials and break them down.
Those that produced these beta-lactam enzymes therefore survived and became resistant to further attacks and that antibiotic was no longer effective. To counter these beta-lactamase enzymes, compounds were produced to bind to and neutralise these enzymes, beta-lactamase inhibitors and hence the introduction of clavulanic acid in the eighties. This combination has proven highly effective over the last 35 years in both human and veterinary medicine.
Penicillinases were also produced by Staphylococci and a penicillinase-resistant compound was produced, the isoxazolyl penicillin methicillin in 1960. This proved highly effective in man to combat these infections until the Staphylococci found another route of resistance development and that was to change the binding site of the penicillin-binding protein (PBP) in the cell wall, so that the drug could not act on the bacterium and it survived, hence the development of methicillin-resistant Staphylococcus aureus (MRSA), as early as 1968 in man, which has become a major clinical problem in human-hospital medicine and also recently (2006) a major societal problem in EU pig farms, farmers and vets. This resistance mechanism means that all beta-lactam antibiotics are ineffective against MRSA and other families of antibacterials are required e.g. the glycopeptide vancomycin, oxazolidinone linezolid etc. In veterinary medicine, cloxacillin has been used for mastitis treatment in dairy cows, since the seventies with very few reports of MRSA being found in milk.
Streptococci – bacteria thriving in aerobic environments.
A further expansion of the penicillin spectrum of activity was to be effective against Pseudomonas aeruginosa. This is a Gram –ve aerobe and is one of the hardest bacteria to treat in man. It commonly affects people with cystic fibrosis of the lung and the ureidopenicillin piperacillin was one that was developed.
Carbapenems, the current last resort antibacterials in human medicine for Gram –ve infections such as Klebsiella pneumoniae and Pseudomonas, were introduced from 1984. Imipenem and meropenem are examples and have been highly effective until quite recently, when carbapenemase producing resistant strains have developed in the EU, US and Asia in particular. These are not currently approved for use in veterinary medicine.
Cephalosporins
A further development in the beta-lactam class of antibiotics was the introduction of the cephalosporins (see Table 2), which were primarily penicillinase resistant and the first generation had a similar spectrum of activity to the aminobenzyl penicillins ampicillin. Cephalothin was the first one in the sixties and additional ones such as cephalexin and cephradine followed. These are classed as first generation cephalosporins and now there are up to five generations, not so many are used in veterinary medicine but many are used for mastitis in dairy cows.
Double dilution susceptibility testing of bacteria in broth. The third tube on the left shows minimum bactericidal concentration (MBC); the sixth from the left shows the minimum inhibitory concentration (MIC).
There is some cross-over in the generations and there are not too many major differences between the later ones. Ceftiofur (3G) and cefquinome (4G) are the two major injectable products in pigs. There was a major difference in extension of spectrum between the first and third generation cephalosporins and they have become hugely significant in human medicine. It is understandable that there is concern that there may be some cross-resistance spread of extended spectrum beta-lactamases (ESBLs) selected in bacteria from animal use to humans. The degree of spread is probably quite small, but these products should be used judiciously in veterinary medicine. Use in poultry has been stopped in the EU, where most of the ESBLs were found.
Beta-lactamase inhibitors such as clavulanic acid, sulbactam and tazobactam can be used with the cephalosporins to neutralise ESBLs but unfortunately, not all of them, so resistance can be a problem.
This article has focused on the beta-lactam antibiotics because of their importance in human medicine as well as veterinary medicine. The developments and modifications over the years have been ingenious in many ways both in improving the spectrum of activity, changing the mode of actions to attack infections and fighting resistance development. Welcome to the wonderful world of antimicrobials and the beta-lactam antibacterials especially, let us hope that the next decades will bring some startling new additions to help combat the growing resistance issues, especially in man.
For more information on the classification of antimicrobials see David Burch’s blog “The classification of antimicrobials – a clash of views“