MRSA in pigs: A link with cephalosporins?
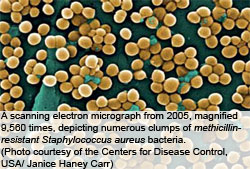
The subject of methicillin resistant Staphylococcus aureus (MRSA) was reviewed a couple of years ago after the last International Pig Veterinary Society (IPVS) Congress. It is timely after the recent Congress in Vancouver (18-21 July 2010), where again it was a hot topic for debate, to summarise the findings to date.
By David Burch, Veterinarian, Octagon Services, Windsor, Berkshire, UK
A great deal of work has been carried out in the last two years. We have had two baseline survey results from EFSA (2009, 2010) on breeder herds (supplying breeding stock) and breeding herds producing stock for finishing and the prevalence within EU countries and inter-country transmission of MRSA. There has also been an important joint meeting of the American Society of Microbiology (2009) and its European counterpart in London on MRSA in animals (including pigs) and its public health implications, as well as several new publications.
EU survey results
In survey A (EFSA Journal, 2009), 1,421 holdings mainly supplying breeding stock and 3,176 farms with breeding animals for fattening were tested using pooled dust samples for the presence of MRSA. This covered most of the EU member states (24) and 2 non-EU countries. The EU prevalence in breeding farms was 14% but in breeding/finishing or production farms 26.9% (see Figure 1).
There was much inter-country variation but only seven members did not find MRSA in either their breeding or production units and fortunately the UK was one of these. Spain, Germany, Belgium and Italy were the highest and surprisingly, the Netherlands was below the EU average, as this is where the initial problem was identified and investigated. The clonal type of MRSA was primarily ST398 (92.5%) formerly associated with livestock but in Italy and Germany, predominately, additional types were found associated with cattle and humans.
The second set of results from report B (EFSA, 2010) looked at risk factors for MRSA contamination of breeding and production holdings. The main risk associated with both farms was size. As units increased in number of breeding pigs, so they had a higher chance of contamination with MRSA. It was not clear whether this was due to a within-holding diffusion of MRSA due to management techniques or a greater risk of introduction through a higher level of introduction of replacement breeding stock. The risk varied between countries, irrespective of breeding herd size, depending on prevalence in the country.
The spread by the breeding pig trade was also investigated. There was a strong association between the prevalence of MRSA in breeding herds and the prevalence in production herds – i.e. there is a high chance of vertical transmission from infected breeding stock. This was also strongly demonstrated by inter-country importation of MRSA contaminated breeding animals. This is a highly significant confirmatory finding – if you don’t want MRSA don’t buy contaminated breeding stock. Farmers and vets must insist on checking a breeder supplier’s MRSA status before purchase.
Tenhagen and others (2010) from Germany also found buying pigs from several different weaner and grower farms also increased the risk of MRSA introduction into finisher farms.
Some lobbyist organisations have criticised the results, especially for the UK being zero, saying the sampling method from pooled house dust was not accurate enough and that individual, nasal swabs should have been used. This would have added a significant cost to the whole exercise and also Schulz and others (2010) at the IPVS showed that pooled dust samples were 78% accurate in comparison with nasal swabs for the isolation of MRSA, thereby confirming the relative accuracy of the test and the validity of the result.
MRSA worries?
In many respects, both in pigs and man it has proven a relatively minor clinical problem. There have been descriptions of disease in Denmark with ST398 (Larsen and others, 2009). In the period of 2003-08 it was detected in 109 people and 35 (32%) had an infection at the time of detection. These were superficial skin and soft tissue infections but two cases were severe, one involving arthritis and organ failure and one pneumonia in a new-born child. In Germany, Koeck and others (2010) found 1695 isolates of MRSA in humans in North Rhine- Westphalia, a pig-dense part of Germany, in routine screening. Of these 305 (18%) were associated with ST398 but of the 38 samples found in blood cultures (bacteraemia) only 1 (2.6%) was ST398. Therefore, there is a potential risk of disease in humans but it is considered low in comparison with hospital-acquired and other community acquired MRSA infections.
In the EFSA report (2009) they refer to the infection as an ‘occupational health risk’ for farmers, veterinarians and their families. Cuny and others (2009) from Germany showed that from 113 farmers/workers that were directly exposed, 97 (86%) had nasal colonisation with MRSA but of the non-exposed family only 4.3% were positive. At the local school only three children were positive (0.6%) but all three were from pig farms in the area. Veterinarians attending pig farms also had a high prevalence of 45% but the 9% non-exposed family members were found to be colonised. In slaughterhouses 5.6% of workers operating in the live animal section were reported positive for MRSA (Van Cleef and others, 2009). Although the remaining sections of the slaughterhouse were contaminated, no other workers were found to be positive.
EFSA was correct that it is an occupational health risk particularly for those in direct contact with pigs but the risk subsides rapidly the further away a person is from the source, until it is almost zero for the general population.
Spread within the herd
Weese and others (2009) from Canada looked at the infection of piglets in a longitudinal way over ten weeks. A batch of ten mixed MRSA positive and negative sows was reared together and both groups of piglets gradually became colonised with time (see Figure 2), peaking at six weeks of age. Harper and others (2009) from Iowa, US showed in a small survey of 13 farms that MRSA could be found in 57% of confinement herds, whereas none of the organic herds were infected. In a larger survey, Blaha and others (2010) in Germany showed that 79% of conventional herds were MRSA positive and only 15% of organic herds but wild boars were free. In the UK, 42% of sows are kept outdoors and this might also be an important factor.
Antimicrobials
When it comes to antimicrobial use and MRSA, it becomes hugely political and sometimes science is overwhelmed. On one side, there is a fear of MRSA from the human hospital stories and therefore to see an explosion of MRSA in livestock is an obvious concern. However, it is being used as an excuse by some to blame all veterinary antibiotic use for the problem, particularly in pigs.
Methicillin resistance confers resistance against all of the penicillins, synthetic penicillins (amoxycillin) and all generations of cephalosporins (in that order) by genetically altering the penicillin-binding proteins where these drugs act. Methicillin and related compounds are not used in pig medicine. If one looks at what the likely selectors for MRSA are, it is likely to be the third and fourth generation cephalosporins, which select for MRSA strains. The third generation cephalosporin most commonly used in pig medicine is ceftiofur by injection. In some countries like Germany (Pabst, 2009), it is widely used in piglets for the treatment and prevention of respiratory infections and arthritis, primarily associated with Streptococcus suis, as well as respiratory infections associated with Actinobacillus pleuropneumoniae, Pasteurella multocida and Haemophilus parasuis.
The long-acting formulation is ideal for piglets, as it provides nearly seven days protection. It does not have a specific indication for S. aureus and the development of resistance to it can be considered an inadvertent adverse event, but one that is well recognised in human medicine and possibly foreseen in veterinary medicine too.
Standard antimicrobials
Other countries, like the Netherlands (Van Duijkeren and others, 2008) looked at farms, their medication and the number of MRSA positive pigs and concluded that the use of standard antimicrobials seemed to be a risk factor. On closer scrutiny and if one took out the use of amoxycillin and ampicillin from the equation, which averaged a 74% MRSA resistance, the use of trimethoprim/sulpha, colistin, tulathromycin, tylosin, tetracycline and doxycycline had an average of 27% resistance and no medication was 10%. Although amoxycillin and ampicillin are not considered selectors of MRSA resistant strains, they would be expected to kill susceptible strains and thereby increase MRSA prevalence.
Another survey (Tenhagen and others, 2010) suggested that antibiotic use increased the risk of herds being positive. The main products used were tetracyclines (28% of herds), amoxycillin (20%) and tylosin (18%). However, Brons and others (2010) from the Netherlands reported that antimicrobial use and MRSA on a farm were not significantly associated but that larger farms tended to use more antimicrobials on a group basis. Neither survey had looked at piglet injections or ceftiofur use but only in-feed or in-drinking water antibiotic use.
Aarestrup and others (2010) from Denmark, looked at the susceptibility/resistance profiles of 31 MRSA and 24 MSSA (susceptible) ST398 isolates to commonly used antibiotics and zinc chloride (see Table 1). The resistance patterns were fairly similar for erythromycin and tetracycline and therefore were thought unlikely to be associated with the methicillin-resistance gene mecA but there was a difference regarding zinc, where the MRSA isolates showed a 74% resistance. He postulated that zinc use in feed may have contributed to the emergence and further spread of ST 398. Medical authorities recently reviewed this in the UK and although metallo-resistance genes have been associated with a different type of resistance gene (extended-spectrum beta lactamases or ESBLs) in gram negative bacteria, such as E. coli, they have not been found in human MRSA, but possibly nobody has looked. It was thought that while most of the UK pig population receives zinc in its feed at weaning and MRSA have not been found that it is an unlikely direct selector for MRSA but might be associated with the mecA gene or other genetic/plasmid material, as MRSA tend to demonstrate multi-resistance. Further work comparing Dutch MRSA/MSSA isolates would be of interest, as officially zinc oxide is not used at high levels in the Netherlands although lower nutritional levels are administered.
In conclusion, much work appears to have been carried out on MRSA over the last two years. The prevalence across Europe and N. America is high and mainly associated with the ST 398 clone. China is seeing a different clone, ST9. The cause of resistance selection appears to be primarily associated with the use of third and fourth generation cephalosporins and not other antibiotics. The risk to the general public is low but to pig farmers, vets and slaughter house workers it is significant. This has whipped up a political debate, with the UK planning to stop advertising antimicrobials to pig farmers and the EU examining antimicrobial use on a wider scale. There were no reports on how to get rid of the infection once acquired, which was disappointing, but does leave prevention as the best form of defence and also not to buy stock whether for breeding or for finishing from MRSA-infected sources – this applies both at a farm and national level.











