Detecting ileitis in a swine herd

Ileitis is an inflammation of the small and large intestines caused by an infection with the bacteria Lawsonia intracellularis. The gold standard to diagnose this disease has long been to detect Lawsonia with a specific stain in the ileum. Recently, more insights have become available about alternative diagnostic methods, using highly sensitive qPCR techniques.
Ileitis is an intestinal disease leading to huge economic losses in pig production which is caused by the bacteria Lawsonia intracellularis. As feed constitutes the highest costs in pig production, currently over 70% of the variable cost price in pig production, a perfectly working digestive system is pivotal for profitable pig production. Even infections with low amounts of these bacteria, lead to production losses, like a lower average daily gain (ADG) and a higher feed conversion ratio (FCR).
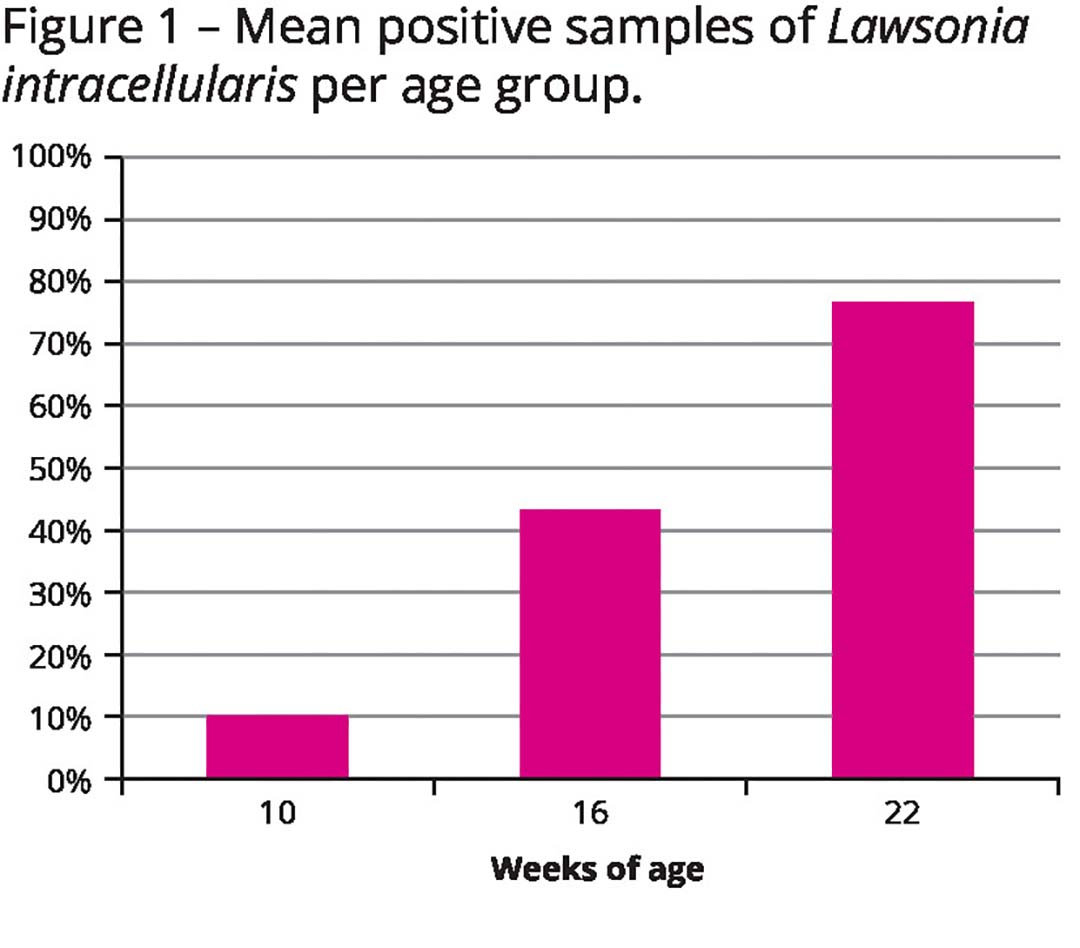
While ileitis is frequently associated with diarrhoea, the disease is not clinically visible in most cases, which makes it hard to diagnose it. When focusing on serology, we see positive farms on a wide scale. In general, 80% of the pigs at slaughter age are antibody positive, even in high health production systems. It’s not possible to connect the antibody status to a loss of production.
Gold standard
The gold standard to diagnose ileitis is by looking at a piece of ileum, the last part of the small intestine, with a microscope to confirm the presence of the typical lesions associated with the disease. By using immunohistochemistry, a specific staining process, the presence of the infectious L. intracellularis together with the ileum lesions confirms the diagnosis. That requires sacrificing animals for necropsy. But without the ability to identify clear ileitis suspected cases, or instance a lack of diarrhoea, to better target samples a lot of animals have to be evaluated (at least 30) which under practical circumstances cannot be done due to the high cost in euthanised pigs.
Alternatively, in recent years, a lot of focus has been set on checking rectal shedding of L. intracellularis. By routinely checking the faeces and/or oral fluids, subclinical infection can be found.
The fact that pigs do not shed continuously complicates this type of diagnostics, as well. In general, 85% of the randomly tested samples lead to negative results. Even in challenge studies in which pigs are infected with huge loads (billions) of bacteria, infected pigs only consistently shed for a small number of days. That lack of sensitivity could be compensated for by taking more samples, which can be pooled as well to save on diagnostic costs.
Serum antibody testing
Serum antibody testing of the population might be another option. Taking a closer look at antibodies and how the positive pigs are distributed amongst the different age groups, the same consistent trend can be seen all over the world. Most infections start in the grower phase and the disease spreads slowly in infected herds as age increases. And with 20% of the animals not having seroconverted at market age, it would still be likely to find active infections in a proportion of the pigs at slaughter. During the slaughter process, it would be easy and affordable to take a small sample from the ileum, without any loss of carcass value.
Confirming the presence
To confirm the presence of disease at slaughter, between 2018 and 2020 a Boehringer Ingelheim team in the Netherlands – and after COVID-19 also including Belgium – monitored a batch of pigs which had been confirmed with subclinical ileitis during the first 4 to 6 weeks of the grow-finish period. At slaughter, 60 ilea were sampled. Almost all these ilea were positive, and the team could establish a correlation between the gold standard microscopic evaluation (expensive and time consuming) and qPCR testing (fast and relatively affordable) of the same tissue samples.
Consequently, next steps were to evaluate the presence of disease on a larger scale by testing over 70 production sites in Europe. Out of these analysed farms, over 60% turned out to have affected ilea at slaughter. In a batch of positive pigs at slaughter, most cases had at least 50% positive ilea out of ten ilea sampled.
Even in cases where pigs were not consistently shedding L. intracellularis in the faeces, those ilea could be found positive at slaughter. That indicates that diagnosing subclinical ileitis at slaughter has a higher sensitivity than when compared to random faecal sampling in the barn. Current findings demonstrate that taking ten random ilea samples at slaughter confirms whether or not a batch of pigs suffers from subclinical ileitis.
Another lesson learned during the evaluation of ilea at slaughter, is that in mild cases, the naked eye cannot tell the difference between affected and healthy tissue. It should be confirmed using qPCR, to measure the impact of this ubiquitous disease on productivity.
Pooling ileum samples
With pooling these ileum samples for PCR analysis, it is possible to reliably confirm subclinical ileitis in a herd for a fraction of the costs involved using random testing of faeces or oral fluids. That, in turn, can increase the speed of decision-making on whether to implement an ileitis control programme with oral vaccination. As a result, what can be avoided are adverse effects like huge negative impacts of subclinical ileitis like a drop of ADG and increased FCR.
Oral vaccination against ileitis has shown to reverse those negative effects. In a compilation of 38 studies, oral vaccination under field conditions improved ADG by 38 g, reduced FCR by 0.08 and reduced mortality by 0.8%. The FCR improvement results in over 7.5 kg less feed consumed per pig, which is a saving of € 2.36 assuming feed prices are € 15/ton (like in winter/spring 2024). Due to an improved microbiome induced by the oral vaccination, other intestinal threats like Salmonella are reduced as well. Oral vaccination is safe without side effects, not losing a single day of productivity to get the maximum results out of a finishing pig herd.