BLOG: Antibiotic surveys and their significance?
We have recently completed a survey of antimicrobial usage in the UK. Following on from this, I have tried to establish the usage of cephalosporins in pigs and their comparative impact on resistance in pig pathogens and potentially human pathogens.
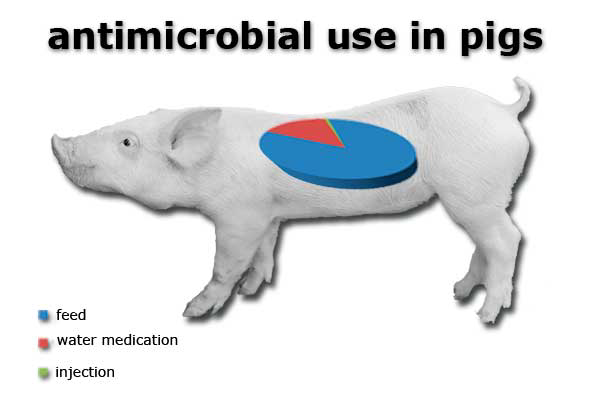
BPEX, the UK pig levy-payers association recently sponsored a survey of antimicrobial use in pigs in the UK (Burch, 2014). It showed that approximately 167 tonnes of antibiotic were used for pigs in 2012, approximately 41% of overall antimicrobial use. The majority of this use was in feed (84.5%) followed by water medication (15%) and by injection (0.8%) or 1.3 tonnes. This got me thinking, if we are using so little by injection what is the likely usage of cephalosporins in UK pig production, especially, as this is one of the critically important human antibiotics and what impact is it having on antimicrobial resistance selection in pigs and potentially man?
According to our Veterinary Medicines Directorate data (VMD, 2013) the sales of beta-lactam antibiotics (penicillins and cephalosporin based products) is 82 tonnes (20%) of a total of 409 tonnes and cephalosporins is 6.9 tonnes of that figure, in both farmed and pet animals. Human use of antibiotics by comparison in the UK is approximately 458 tonnes in total; beta lactams and cephalosporins are 310 tonnes (68%) and included in that figure is 45 tonnes of cephalosporins (VMD, 2010) both in the community (32 tonnes) and hospitals (13 tonnes), hence their significance.
The main cephalosporin used in pigs is ceftiofur, a 3rd generation cephalosporin, both in short-acting and long-acting formulations by injection only. By examining sales and usage data of these products from the survey it can be estimated that approximately 15-20kg of cephalosporin only is used, a minor fraction (0.27%) of total cephalosporin usage in animals, including pet animals and 0.04% equivalent of human use – miniscule.
If one looks at the direct effect of 3rd generation cephalosporins on antimicrobial resistance of bacteria from pigs a very low level of resistance is found, even in clinical isolates (see Table 1). This is in comparison with ampicillin, where a high level of resistance is seen in enteric infections such as E. coli and Salmonella spp but fortunately not against respiratory bacteria such as P. multocida and A. pleuropneumoniae. The combination of amoxicillin+clavulanic acid, the latter which is a beta-lactamase inhibitor to reduce resistance caused by beta-lactam enzyme producing bacteria to destroy the antibiotic, shows marked reduction in resistance levels. Cephalosporins as a group are mainly resistant to simple beta-lactamases, hence the attraction to use them but select for bacteria producing extended-spectrum beta-lactamases (ESBLs), which is of major concern in human hospital medicine.
Table 1. Susceptibility of various pig bacteria to ampicillin, amoxicillin/clavulanic acid (beta-lactamase inhibitor) and 3rd generation cephalosporins (cefpodoxime mainly and ceftazidime against Salmonella spp*) (VMD 2013).
Ampicillin resistance and cephalosporin resistance seem to be higher in baby piglets, where these antibiotics are regularly used, especially for Streptococcal infections and the E. coli in the gut have responded and selected for resistance. Cephalosporin resistance mainly disappears as the pigs get older. Some Salmonella spp are also showing a very low level of resistance (4/569 isolates).
In comparison with human antimicrobial resistance in England (VMD, 2010) against E. coli, which caused bacteraemia (found in the blood) a potentially life-threatening infection, 61% were resistant to ampicillin/amoxicillin, 20% to amoxicillin+clavulanic acid and 11% to ceftazidime, a 3rd generation cephalosporin.
Surveys of the correlation of antimicrobial usage and surveillance of bacterial resistance data can give some very useful information regarding what is likely to cause antimicrobial resistance. The use of some antibiotics such as ampicillin/amoxicillin is very common, so resistance development is likely to be high, whether in humans or in animals. Similarly for cephalosporins, if they are widely and directly used in a population, then it can be expected that they will select for resistance such as ESBL production as well.
On European Antimicrobial Awareness Day it might be worth reminding both sides of the debate, medical and veterinary, to use antimicrobials as responsibly as possible to minimise resistance development.











